Cook County Health is Making an Impact.
As part of our mission to elevate the health of Cook County, we strive to do more than provide care in our communities.
Now more than ever, we’re committed to using our voice to raise awareness on the issues that impact our homes, our neighbors and our communities locally and nationally. Our goal is to bring real issues to light, create a forum for conversation and provide solutions to impact change.
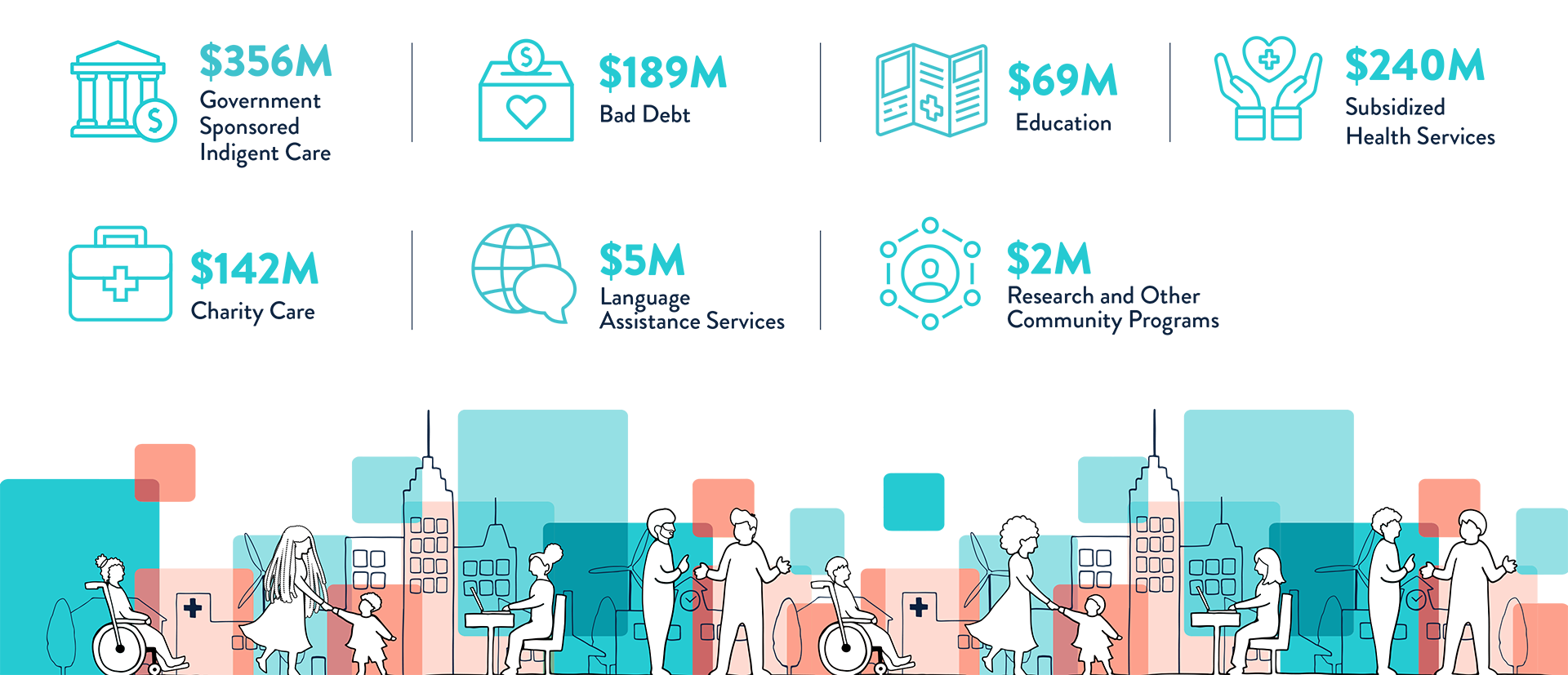
Community Benefits
Cook County Health is proud to invest in the health of those whom we serve.
We do this by providing free and discounted medical care, offering public health services, funding community-based resources, educating the next generation of health care providers and more.
In all, Cook County Health provided $1 billion in community benefits in 2022.
Definitions
Bad Debts
The bad debt expense resulting from the extension of credit for services the hospital provided for which payment was expected but not received.
Donations
Cash and in-kind donations such as the value of meeting space, equipment, and personnel to assist other community health care providers, social service agencies and organizations.
Education
Costs incurred for hospital-based educational programs such as medical residency and internships and nursing. radiology technician and physical therapy programs, reduced by direct medical education funding from third-party payer reimbursement, offsite rotation revenue, fees charged, etc. Community health education and wellness programs should be reported under Subsidized Health Services section.
Government Sponsored Indigent Health Care
Unreimbursed cost of Medicare, Medicaid, and other federal, State, or local indigent health care programs, eligibility for which is based on financial need. Includes both inpatient and outpatient services. In calculating this cost, hospitals should apply a total cost-to-charge ratio to obtain costs, unless the hospital has an alternative method for determining costs, then deduct any revenues that were received for such services.
Language Assistant Services
Unreimbursed actual costs pertaining to language assistance service such as salaries and benefits of translators, costs of translation services provided via phone and costs of forms, notices and brochures provided in languages other than English, offset by any revenue received for these services.
Research
Cost of research activities conducted primarily to advance medical or health care services, including clinical drug trials, demonstration projects for alternative delivery systems, disease-specific research, etc. This portion of the report should include only actual costs not covered by grant funding or donations.
Subsidized Health Services
Subsidized health services for which the hospital, in response to community need, must subsidize from other revenue sources. It includes, but is not limited to, such services as emergency and trauma care, neonatal intensive care, community health clinics, and collaborative efforts with local government or private agencies to prevent illness and improve wellness, such as immunization programs. Includes specialty services that yield a financial loss such as rehabilitation, burn care, substance abuse, HIV/AIDS, geriatric, pediatric, clinics, hospice, physician referral service, ambulance and programs to prevent illness or injury and improve wellness such as community health screenings, immunization programs, health education, counseling and support groups, poison control, etc. Hospitals should determine the financial loss by calculating the costs of staff, materials, equipment, space, etc., offset by any third-party payment, patient fees, or donations.
Volunteer Services
Voluntary activities provided by hospital employees and volunteers in connection with a hospital’s Community Benefits Program that take place as the result of a formal hospital initiative to organize or promote voluntary participation in the activity. Value of volunteer time is to be calculated as the number of volunteer hours multiplied by minimum wage.
ON THE FOREFRONT OF GROUNDBREAKING RESEARCH
ON THE
FOREFRONT OF
GROUNDBREAKING RESEARCH
COOK COUNTY HEALTH IS LEADING THE PACT.
Cook County Health, along with all Level 1 trauma centers in Chicago and emergency centers nationwide, is participating in a Department of Defense funded trauma study titled the Prehospital Airway Control Trial (PACT).


Over the next four years, this trial will compare two emergency breathing techniques to see if one helps trauma patients.
The study is conducted under Exception From Informed Consent (EFIC). This means that trauma patients over the age of 15 who cannot breathe will be automatically enrolled in the study. The patient or immediate family will be informed as soon as possible and will have the opportunity to decide if they want to continue the trial.
Check out our Research page to learn more.
Don’t Get
Sick This
Flu Season


3 Ways to Prevent the Flu
Get the flu vaccine
Stop the spread of germs
-
Wash your hands regularly
-
Cover your nose or mouth when coughing or sneezing
-
Clean and disinfect surfaces in your home – like door handles and countertops
Stay home when you’re sick
Avoid close contact with anyone who is sick. If you get the flu or feel unwell, stay home from work or school so you don’t spread illness to others.
5 Flu Myths DEBUNKED
The flu vaccine will give you the flu.
Healthy people don’t need to be vaccinated.
FACT: Everyone older than 6 months should get vaccinated, especially young children, babies, pregnant women, seniors and people who have chronic illnesses. When everyone is vaccinated, it helps the whole community stay healthy.
The flu is just a bad cold.
You can’t spread the flu if you’re feeling well.
You don’t need a flu shot each year.

THE

OF THE MATTER

Heart disease is the leading cause of death for men & women.
Prediabetes is a serious health issue, where blood sugar levels are higher than normal.



Heart disease and diabetes are linked. Both are manageable and preventable.
Diabetes affects some communities more than others. African American and Latino people are 2-3 times more likely to have diabetes.
3 tips to prevent heart disease and diabetes:
Stop smoking
See your doctor for regular checkups
Eat healthy foods, like fruits and vegetables
Transforming Cook County Health

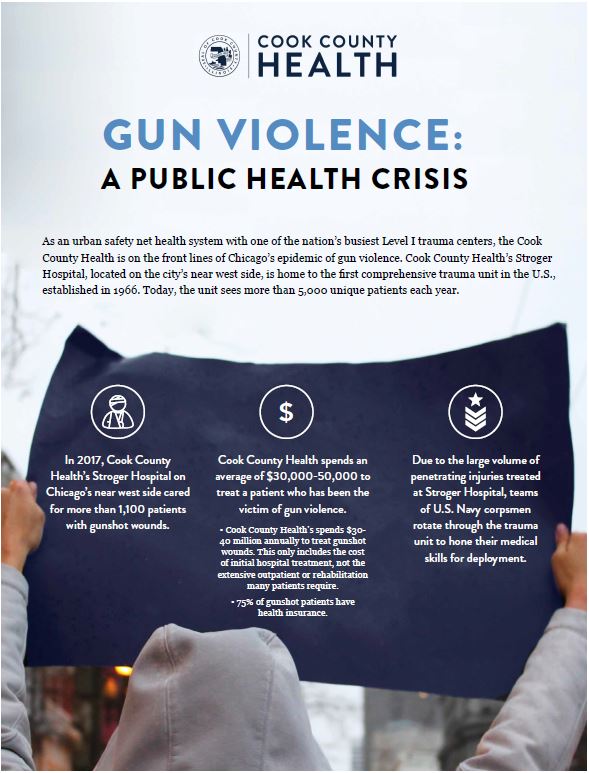
Gun Violence
As an urban safety net health system with one of the nation’s busiest Level I trauma centers, Cook County Health is on the front lines of Chicago’s epidemic of gun violence.
More than 1,000 people have been shot in Chicago in 2018. Despite Chicago and Illinois having some of the strictest gun laws in the U.S., it continues to be the epicenter of this modern public health epidemic. The experience in Chicago and Illinois demonstrates why state-by-state laws are not sufficient and why we need federal gun control laws.
Cook County Health supports common sense gun regulations and other measures to combat the mortality and morbidity caused by firearms, including:
Banning high-capacity automatic/semiautomatic firearms, bump stocks and silencers
Strengthening permits and universal background check requirements for all gun owners, including mandatory training and a waiting period
Requiring anyone who sells a gun to have a dealer license
Requiring reporting of a lost or stolen gun within 48 hours
Funding research on gun violence to develop public health interventions
Investing in trauma informed care services to support victims of gun violence in their recovery
Media Highlights
Hundreds of thousands march in Washington for gun control
Chicago county health system calls for federal gun control
Chicago students in city, D.C. prepare for March for Our Lives 2018 rally
Shot on the streets of Chicago as teens, they’re heading to D.C. to protest gun violence
We have nothing to lose
Beyond gun control, student marchers aim to upend elections
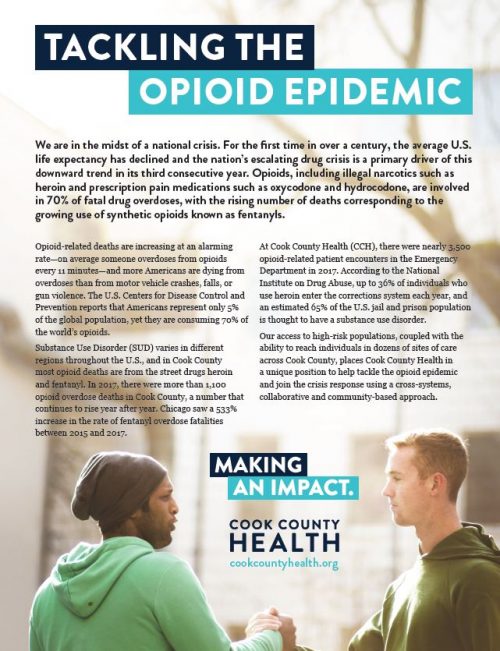
Opioid Use
The U.S. is facing an opioid epidemic, and Cook County is not immune. In the last decade, opioid use and abuse has skyrocketed, becoming a public health crisis that shows no signs of slowing down.
Cook County has embarked on a number of initiatives to combat the epidemic of opioid use:
In 2017, Cook County Health received $2.6 million to establish new pilot programs to fight the county opioid epidemic. Programs will include a second Community Triage Center, expansion of the system’s medication assisted treatment options and case management services, and new fentanyl screening capabilities. Funding in support of these initiatives was awarded to Cook County Health by the Illinois Department of Human Services, Division of Alcoholism and Substance Abuse (IDHS-DASA). These funds are part of an Opioid-State Targeted Response (STR) grant award (TI-080231) to IDHS-DASA from the U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration as part of the 21st Century Cures Act.
Cook County Health currently offers medication-assisted treatment (MAT) at most of its community health centers and is actively working to expand access throughout its clinic network and through partnership with community treatment providers.
Stroger Hospital has launched a pilot program to initiate MAT in the Emergency Department in coordination with addiction medicine providers to reduce the risk of overdose and attrition between an ED visit and an outpatient appointment with a substance use specialists.
Through Cook County Health Cermak Health Services at the Cook County jail, detainees with a history of opioid use are offered training and naloxone upon release to reduce the incidence of post-detox overdose.
Cook County Health partners with three community health centers – Esperanza Health Centers, PrimeCare Community Health, and Heartland Health Centers – to offer medication-assisted treatment for opioid use disorder within their primary care clinics.
Cook County Health and CCDPH are working with medical providers to improve and develop safe prescribing protocols, including an annual training module.
CCDPH facilitates a panel of opioid addiction experts to provide awareness and education training on opioid addiction throughout the community as well as its own workforce.
Click on our white paper below to learn more about how Cook County Health is addressing the opioid epidemic.
Media Highlights
How Chicago hospitals are addressing the opioid epidemic
New opioid addiction treatment offers hope at Cook County hospitals
4 ways Cook County Health and Hospitals System is addressing opioid addiction
City Club of Chicago opioid epidemic panel
Officials warn of new deadly opioid
Heroin’s colorblind, gender-equal, easy-access assault on America
Behind the epidemic of opioid abuse in the U.S.
Treating the community: Cook County Health CEO Dr. John Jay Shannon answers 5 questions on the opioid epidemic
Over 40 Cook County overdose deaths linked to new opioid
Fentanyl derivative causing more overdose deaths
Elephant tranquilizer carfentanil causes first death in Chicago area
Suicide
Suicide continues to be a leading cause of death for Americans, taking a life every 13 minutes, according to the Centers for Disease Control and Prevention (CDC). Cook County Health would like to encourage residents to know the importance in recognizing the warning signs in others.
“Suicide is rarely caused by a single factor,” said Dr. Diane Washington, executive director of behavioral health at Cook County Health. “Many people who do not have a mental illness can still suffer profoundly after a break-up, job loss or a health scare. We should reach out to someone who might be struggling to lend a hand in support.”
Although more than 50% of those who commit suicide reportedly have not attained any psychiatric diagnosis, more than 90% of people who commit suicide are found to have at least one mental health disorder such as depression, anxiety disorder or bipolar disorder, according to the American Foundation for Suicide Prevention.
There are effective treatments, like medication and therapy with a mental health professional, to address some of the underlying health issues that put people at risk for suicide.
Despite this, suicide rates continue to increase in the U.S..
Here are suicide warning signs:
Talking about wanting to die or researching ways they can kill themselves
Talking about feeling hopeless, trapped or being a burden to others
Increasing drug or alcohol use
Extreme mood swings
Getting too much sleep or too little
Isolating themselves from activities or groups they used to be involved in
Everyone can help prevent suicide by learning the warning signs, removing firearms, medications and other potential tools for suicide among people at risk and contacting the National Suicide Prevention Lifeline for help. The National Suicide Prevention Lifeline at 1-800-273-TALK (8255) is a confidential, toll-free number to people considering self-harm. It is available 24 hours a day, 7 days a week.
In addition, CCH’ Community Triage Center (CTC) in Roseland provides evaluation, crisis stabilization and treatment for patients presenting with psychiatric and/or substance-related crises 24 hours a day, 7 days a week. To make an appointment with a mental health professional at Cook County Health, you can also call 312-864-0200.
Metropolitan Chicago Breast Cancer Task Force

Cook County Health and other area hospitals have joined the Metropolitan Chicago Breast Cancer Task Force to close the gap in breast cancer mortality rates between African-American and white women.
From 2006 to 2013, a 2017 study published in Cancer Causes & Control showed that the mortality rate from breast cancer among black women dropped by 13.9 percent, driving it below the national average.
The results were so dramatic that the Chicago Department of Public Health gave the Murphy’s group and its partners –– Cook County Health and Hospital System; Rush University Medical Center; Mile Square Health Center; Sinai Health System and Centro Comunitario Juan Diego –– $700,000 to expand their model, which had been credited nationally for the success. The task force is housed at Rush.
Overall, the goal is to take aim at what experts call structural inequities in the quality of care black women receive.